7 Details Therapists Notice About Aged Care Furniture That Others Don’t

When I walk through an aged care home with a therapist, I’m always reminded of one thing: they see furniture very differently to the rest of us. Where a manager may see a comfortable armchair or a tidy dining space, a therapist sees mobility risks, pressure points, transfer pathways, and the subtle ways furniture either supports or hinders a resident’s independence.
Those insights are invaluable — and often the difference between a home where residents move comfortably and confidently, and a home where staff face avoidable challenges every day.
Here are seven small but important details therapists immediately notice about aged care furniture, and how you can use these insights to improve comfort, safety, and functionality across your facility.
1. Seat Height That’s a Few Centimetres Off
A chair that is slightly too low or too high can completely change a resident’s ability to stand safely. When therapists assess seating, the very first thing they notice is whether the seat height supports a safe and effortless sit-to-stand movement, because even a few centimetres can dramatically change the way a resident transfers.
Therapists look for:
-
Whether knees sit higher than hips
-
How much effort a resident needs to stand
-
Whether staff must physically assist every time
Why it matters:
Incorrect seat height leads to more falls during sit-to-stand, increases carer strain, and reduces a resident’s independence.
Manager tip:
Create a simple internal guideline that sets out acceptable seat-height ranges for different resident groups (for example, 430–480mm for general use, higher for residents with reduced lower-limb strength). When trialling furniture, ask your supplier to bring in at least two height options so staff and therapists can directly compare. Make sure your team checks whether residents can stand without rocking forward, pulling on furniture, or needing two-person support. If seat height varies across your home, consider phasing in new pieces with consistent measurements to reduce transfer risk and manual-handling strain.
2. Seat Depth That Causes Sliding or Slumping
Therapists immediately notice whether the resident can sit fully back into the chair without losing their posture. One of the quickest red flags for therapists is whether the seat depth matches a resident’s body size, because an ill-fitting seat immediately forces a resident into sliding, slumping, or perching at the edge.
Therapists look for:
-
Residents perched on the edge
-
Residents sliding forward
-
Excess pressure on the lower spine
Why it matters:
Poor seat depth contributes to back pain, fatigue, pressure injuries and postural decline.
Manager tip:
Always request the seat-depth measurement whenever you evaluate a new chair, not just the width or height. Bring a resident or therapist into the trial process to test whether feet can sit flat on the floor while the resident’s back is fully supported. For lounges and communal seating, consider mixing a few shallower seats into the layout so shorter residents have accessible options. Keep a note of which chair depths work best for individuals and standardise future purchases around those measurements to avoid postural problems.
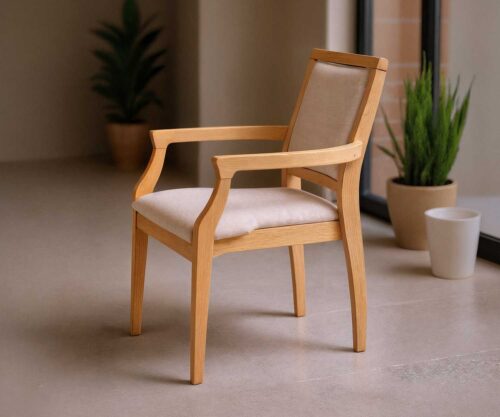
3. Armrest Width and Grip — Not Just Appearance
While armrests contribute to the style of a piece, therapists evaluate whether residents can actually use them to push off or stabilise. Therapists instinctively check whether armrests offer a secure, functional grip, because they know a resident’s ability to push off safely often depends entirely on the shape, strength and spacing of that armrest.
Therapists look for:
-
Armrests that are too rounded
-
Armrests that are too narrow
-
Armrests that flex under weight
-
Armrests set too wide apart
Why it matters:
If residents can’t confidently grip or push from the armrest, transfers become unsafe and assistance becomes mandatory.
Manager tip:
During a furniture trial, ask your supplier to demonstrate the armrest’s stability under downward pressure and sideways leaning — two of the most common ways residents use them. Ensure the armrests are firm enough to take weight but shaped so residents can get their fingers around them securely. It’s also worth checking that staff can safely assist transfers without their hands slipping. When selecting new furniture for dining rooms or lounges, choose chairs with consistent armrest spacing so staff know exactly how to support residents during sit-to-stand.
4. Cushion Firmness and Pressure Distribution
The right cushion feels “comfortable” — the wrong cushion contributes to skin breakdown and unnecessary pain. Before anything else, therapists press down on a cushion to judge firmness and pressure distribution, because they understand how quickly the wrong cushioning can lead to discomfort, instability, or even pressure-related skin issues.
Therapists look for:
-
High-risk residents sitting in soft, sinking cushions
-
Lack of pressure-relieving foam layers
-
Seats that bottom out after a few months
Why it matters:
Furniture cushions are part of your pressure-care strategy. Poor cushioning increases the need for additional equipment, staff monitoring, and wound-care interventions.
Manager tip:
Request detailed information on the foam layers inside each chair — density, firmness, and whether memory foam is included for pressure distribution. During trials, invite your wound-care nurse or therapist to assess whether the cushioning prevents “bottoming out” after a few minutes of sitting. Consider which residents are at highest risk of skin breakdown and prioritise chairs with multi-layered support in high-use areas such as lounges and activity rooms. If cushions are removable, ensure the covers are easy for staff to clean and put back on correctly.
5. Frame Stability During Transfers
Even the most stylish furniture fails if it wobbles during a stand-up. Therapists always test how stable a chair feels under weight, because they know that even a slight wobble can undermine a resident’s confidence and contribute to unsafe transfers.
Therapists look for:
-
Frames that rock or shift
-
Lightweight chairs that slide on flooring
-
Narrow bases that tip when leaned on
Why it matters:
A shaky chair erodes resident confidence and increases the chance of falls.
Manager tip:
Before selecting a new chair or sofa, ask your supplier to show you its internal frame construction and the type of timber or engineered hardwood used. Then physically test the furniture: have staff and therapists lean on it from different angles, mimic a sit-to-stand, and apply lateral pressure to see if anything shifts. In memory support units or high-need areas, prioritise heavier, more stable furniture that won’t slide on vinyl flooring. If your floors are particularly slick, discuss with your supplier whether suitable glides or floor-safe grips can be added.
6. Fabrics That Support Infection Control AND Comfort
Therapists know that a fabric must feel inviting — but also withstand spills, cleaning, and clinical realities. Therapists pay close attention to fabric choice long before they look at colours, because they know texture, cleanability and moisture-resistance directly affect comfort, dignity and infection-control outcomes.
Therapists look for:
-
Fabrics that feel cold or clinical
-
Stitching that traps spills
-
Covers that can’t be spot-cleaned
-
Poor moisture resistance
Why it matters:
The wrong fabric leads to odour retention, staining, and furniture needing early replacement.
Manager tip:
Choose commercial-grade health fabrics with:
-
Heavy-duty rub counts
-
Moisture barriers
-
Antimicrobial protection
-
Texture that feels warm and homely, not institutional
Your supplier should always provide fabric samples to review with your care team.
When selecting fabrics, don’t rely solely on photos — always request swatches and test them in natural light within the home. Run them through your cleaning process: check how easily spills wipe away, whether stains lift, and how fast the fabric dries. Look for commercial upholstery fabrics with moisture barriers and antimicrobial properties, but also check that they feel warm and residential rather than clinical. Make sure your team understands which products are safe to use on the fabric to avoid accidental damage from harsh cleaning chemicals.
7. Clearance for Mobility Devices
Therapists instantly notice when walkers, wheelchairs, or mobility frames don’t fit under or around the furniture. The moment therapists approach a furniture piece, they assess whether mobility devices can fit around, beside, or under it, because poor clearance instantly restricts independence and makes everyday tasks harder than they need to be.
Therapists look for:
-
Dining chairs that block approach
-
Tables residents can’t roll under
-
Lounge layouts that restrict turning circles
-
Gaps that catch wheels
Why it matters:
Poor clearance leads to frustration, crashes, reduced dining independence and increased staff cueing.
Manager tip:
Measure the clearance under your current dining tables and note the dimensions of your residents’ most commonly used mobility devices. Use these figures as non-negotiables when buying new furniture. When trialling a dining setting or lounge layout, bring an actual walker or wheelchair to test access from every angle — not just front-on. Pay attention to turning circles, especially in dining rooms where tight layouts can slow down mealtimes and increase staff workload. A few extra centimetres of space can dramatically improve independence and flow.
The Bottom Line: Therapists See the Hidden Risks (and Opportunities)
Therapists spend every day assessing movement, posture, comfort and safety. They see how furniture affects:
-
resident independence
-
fall risk
-
staff manual-handling strain
-
behaviour and mood
-
overall quality of life
By leaning into their insight early — and selecting furniture designed with therapists in mind — you reduce risk, improve resident comfort, extend furniture lifespan, and create a home where both staff and residents thrive.
Custom Furniture for Aged Care Facilities
Recent Updates
7 Details Therapists Notice About Aged Care Furniture That Others Don’t

When I walk through an aged care home with a therapist, I’m always reminded of one thing: they see furniture very differently to the rest of us. Where a manager may see a comfortable armchair or a tidy dining space, a therapist sees mobility risks, pressure points, transfer pathways, and the subtle ways furniture either supports or hinders a resident’s independence.
Those insights are invaluable — and often the difference between a home where residents move comfortably and confidently, and a home where staff face avoidable challenges every day.
Here are seven small but important details therapists immediately notice about aged care furniture, and how you can use these insights to improve comfort, safety, and functionality across your facility.
1. Seat Height That’s a Few Centimetres Off
A chair that is slightly too low or too high can completely change a resident’s ability to stand safely. When therapists assess seating, the very first thing they notice is whether the seat height supports a safe and effortless sit-to-stand movement, because even a few centimetres can dramatically change the way a resident transfers.
Therapists look for:
-
Whether knees sit higher than hips
-
How much effort a resident needs to stand
-
Whether staff must physically assist every time
Why it matters:
Incorrect seat height leads to more falls during sit-to-stand, increases carer strain, and reduces a resident’s independence.
Manager tip:
Create a simple internal guideline that sets out acceptable seat-height ranges for different resident groups (for example, 430–480mm for general use, higher for residents with reduced lower-limb strength). When trialling furniture, ask your supplier to bring in at least two height options so staff and therapists can directly compare. Make sure your team checks whether residents can stand without rocking forward, pulling on furniture, or needing two-person support. If seat height varies across your home, consider phasing in new pieces with consistent measurements to reduce transfer risk and manual-handling strain.
2. Seat Depth That Causes Sliding or Slumping
Therapists immediately notice whether the resident can sit fully back into the chair without losing their posture. One of the quickest red flags for therapists is whether the seat depth matches a resident’s body size, because an ill-fitting seat immediately forces a resident into sliding, slumping, or perching at the edge.
Therapists look for:
-
Residents perched on the edge
-
Residents sliding forward
-
Excess pressure on the lower spine
Why it matters:
Poor seat depth contributes to back pain, fatigue, pressure injuries and postural decline.
Manager tip:
Always request the seat-depth measurement whenever you evaluate a new chair, not just the width or height. Bring a resident or therapist into the trial process to test whether feet can sit flat on the floor while the resident’s back is fully supported. For lounges and communal seating, consider mixing a few shallower seats into the layout so shorter residents have accessible options. Keep a note of which chair depths work best for individuals and standardise future purchases around those measurements to avoid postural problems.
3. Armrest Width and Grip — Not Just Appearance
While armrests contribute to the style of a piece, therapists evaluate whether residents can actually use them to push off or stabilise. Therapists instinctively check whether armrests offer a secure, functional grip, because they know a resident’s ability to push off safely often depends entirely on the shape, strength and spacing of that armrest.
Therapists look for:
-
Armrests that are too rounded
-
Armrests that are too narrow
-
Armrests that flex under weight
-
Armrests set too wide apart
Why it matters:
If residents can’t confidently grip or push from the armrest, transfers become unsafe and assistance becomes mandatory.
Manager tip:
During a furniture trial, ask your supplier to demonstrate the armrest’s stability under downward pressure and sideways leaning — two of the most common ways residents use them. Ensure the armrests are firm enough to take weight but shaped so residents can get their fingers around them securely. It’s also worth checking that staff can safely assist transfers without their hands slipping. When selecting new furniture for dining rooms or lounges, choose chairs with consistent armrest spacing so staff know exactly how to support residents during sit-to-stand.
4. Cushion Firmness and Pressure Distribution
The right cushion feels “comfortable” — the wrong cushion contributes to skin breakdown and unnecessary pain. Before anything else, therapists press down on a cushion to judge firmness and pressure distribution, because they understand how quickly the wrong cushioning can lead to discomfort, instability, or even pressure-related skin issues.
Therapists look for:
-
High-risk residents sitting in soft, sinking cushions
-
Lack of pressure-relieving foam layers
-
Seats that bottom out after a few months
Why it matters:
Furniture cushions are part of your pressure-care strategy. Poor cushioning increases the need for additional equipment, staff monitoring, and wound-care interventions.
Manager tip:
Request detailed information on the foam layers inside each chair — density, firmness, and whether memory foam is included for pressure distribution. During trials, invite your wound-care nurse or therapist to assess whether the cushioning prevents “bottoming out” after a few minutes of sitting. Consider which residents are at highest risk of skin breakdown and prioritise chairs with multi-layered support in high-use areas such as lounges and activity rooms. If cushions are removable, ensure the covers are easy for staff to clean and put back on correctly.
5. Frame Stability During Transfers
Even the most stylish furniture fails if it wobbles during a stand-up. Therapists always test how stable a chair feels under weight, because they know that even a slight wobble can undermine a resident’s confidence and contribute to unsafe transfers.
Therapists look for:
-
Frames that rock or shift
-
Lightweight chairs that slide on flooring
-
Narrow bases that tip when leaned on
Why it matters:
A shaky chair erodes resident confidence and increases the chance of falls.
Manager tip:
Before selecting a new chair or sofa, ask your supplier to show you its internal frame construction and the type of timber or engineered hardwood used. Then physically test the furniture: have staff and therapists lean on it from different angles, mimic a sit-to-stand, and apply lateral pressure to see if anything shifts. In memory support units or high-need areas, prioritise heavier, more stable furniture that won’t slide on vinyl flooring. If your floors are particularly slick, discuss with your supplier whether suitable glides or floor-safe grips can be added.
6. Fabrics That Support Infection Control AND Comfort
Therapists know that a fabric must feel inviting — but also withstand spills, cleaning, and clinical realities. Therapists pay close attention to fabric choice long before they look at colours, because they know texture, cleanability and moisture-resistance directly affect comfort, dignity and infection-control outcomes.
Therapists look for:
-
Fabrics that feel cold or clinical
-
Stitching that traps spills
-
Covers that can’t be spot-cleaned
-
Poor moisture resistance
Why it matters:
The wrong fabric leads to odour retention, staining, and furniture needing early replacement.
Manager tip:
Choose commercial-grade health fabrics with:
-
Heavy-duty rub counts
-
Moisture barriers
-
Antimicrobial protection
-
Texture that feels warm and homely, not institutional
Your supplier should always provide fabric samples to review with your care team.
When selecting fabrics, don’t rely solely on photos — always request swatches and test them in natural light within the home. Run them through your cleaning process: check how easily spills wipe away, whether stains lift, and how fast the fabric dries. Look for commercial upholstery fabrics with moisture barriers and antimicrobial properties, but also check that they feel warm and residential rather than clinical. Make sure your team understands which products are safe to use on the fabric to avoid accidental damage from harsh cleaning chemicals.
7. Clearance for Mobility Devices
Therapists instantly notice when walkers, wheelchairs, or mobility frames don’t fit under or around the furniture. The moment therapists approach a furniture piece, they assess whether mobility devices can fit around, beside, or under it, because poor clearance instantly restricts independence and makes everyday tasks harder than they need to be.
Therapists look for:
-
Dining chairs that block approach
-
Tables residents can’t roll under
-
Lounge layouts that restrict turning circles
-
Gaps that catch wheels
Why it matters:
Poor clearance leads to frustration, crashes, reduced dining independence and increased staff cueing.
Manager tip:
Measure the clearance under your current dining tables and note the dimensions of your residents’ most commonly used mobility devices. Use these figures as non-negotiables when buying new furniture. When trialling a dining setting or lounge layout, bring an actual walker or wheelchair to test access from every angle — not just front-on. Pay attention to turning circles, especially in dining rooms where tight layouts can slow down mealtimes and increase staff workload. A few extra centimetres of space can dramatically improve independence and flow.
The Bottom Line: Therapists See the Hidden Risks (and Opportunities)
Therapists spend every day assessing movement, posture, comfort and safety. They see how furniture affects:
-
resident independence
-
fall risk
-
staff manual-handling strain
-
behaviour and mood
-
overall quality of life
By leaning into their insight early — and selecting furniture designed with therapists in mind — you reduce risk, improve resident comfort, extend furniture lifespan, and create a home where both staff and residents thrive.